Author: Megan Jones (Adv.Dip.NutMed, BHsc.NutMed)
If you have ever felt ‘butterflies’ in your stomach at the same time as feeling sudden excitement or even a pang of nervousness, you have experienced the gut-brain connection in full swing! Whether we are feeling elated, anxious, sad, or angry, these emotions can all trigger gastrointestinal symptoms, aka a ‘gut feeling’!1
Extensive research in the gut health field tells us that taking steps to improve our gut microbiome through nutrition and dietary changes can positively impact our overall health.2 Did you know that for a healthy microbiome, a wide variety of good bacteria living in our gut is required.3 This can be achieved by consuming nutrient-dense foods that nourish the beneficial bacteria in our gut - promoting their growth and diversity.4
Here, we take a deeper dive into all things gut health, microbiome, vagal nerve and the link between what we ingest and the state of our gut microbiota. We explore how a nutrient-dense diet and nutritional support like Nuzest’s daily Good Green Vitality can boost our microbiome diversity and support our body’s biochemistry to bring us back to balance.
Key takeaways:
- The state of our gut microbiome can be heavily influenced by our genetics but also by our daily food choices.5
- The microbiota (aka ‘gut bugs’) help to digest food and absorb nutrients and help to fight off infection – keeping our bodies functioning optimally.6
- Our gut microbiome can regulate our brain and behaviour via communication along our ‘gut-brain axis’.7
- Nutrients like fibre, along with pre- and probiotics support a healthy and robust gut microbiome.8
What is the gut microbiome?
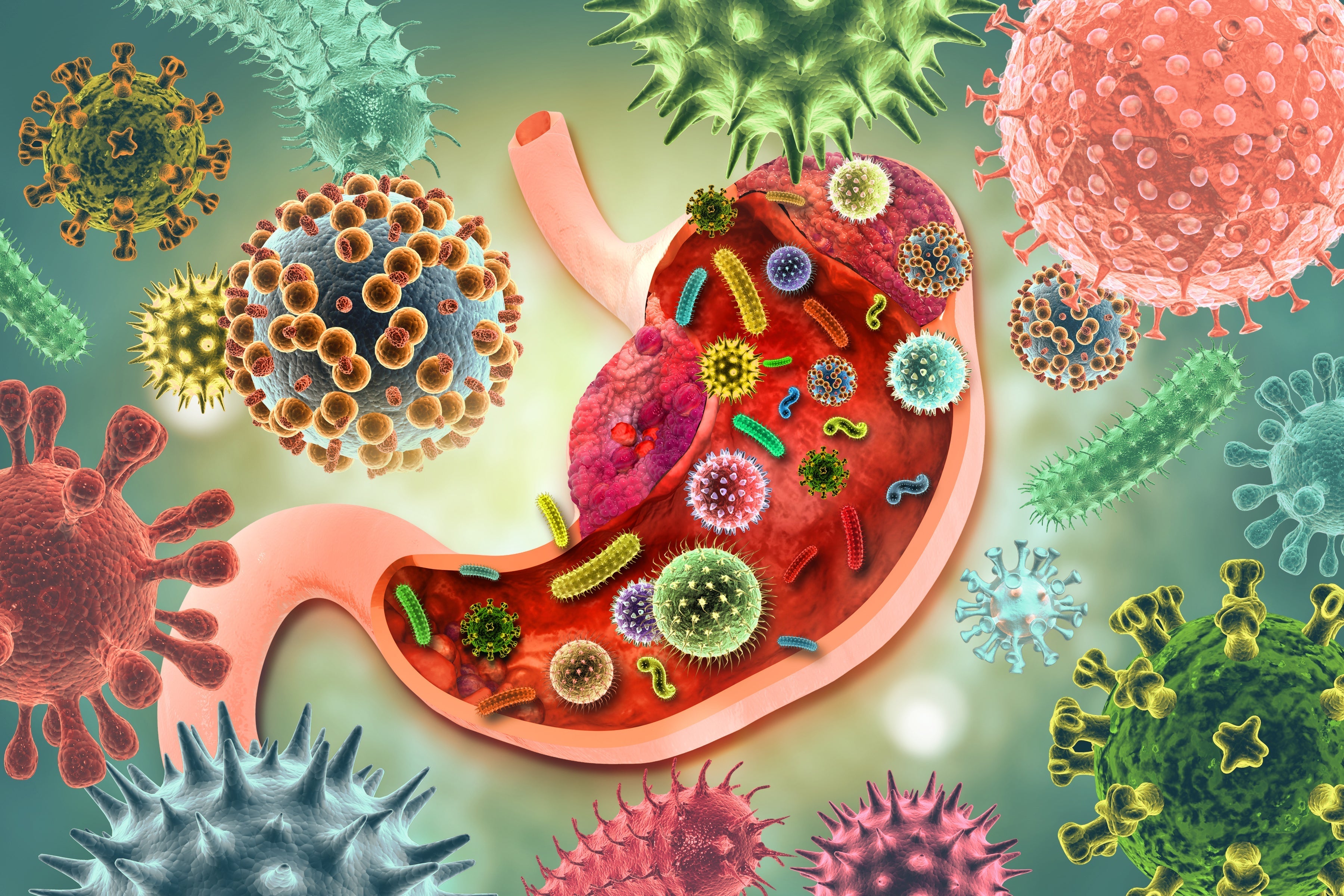
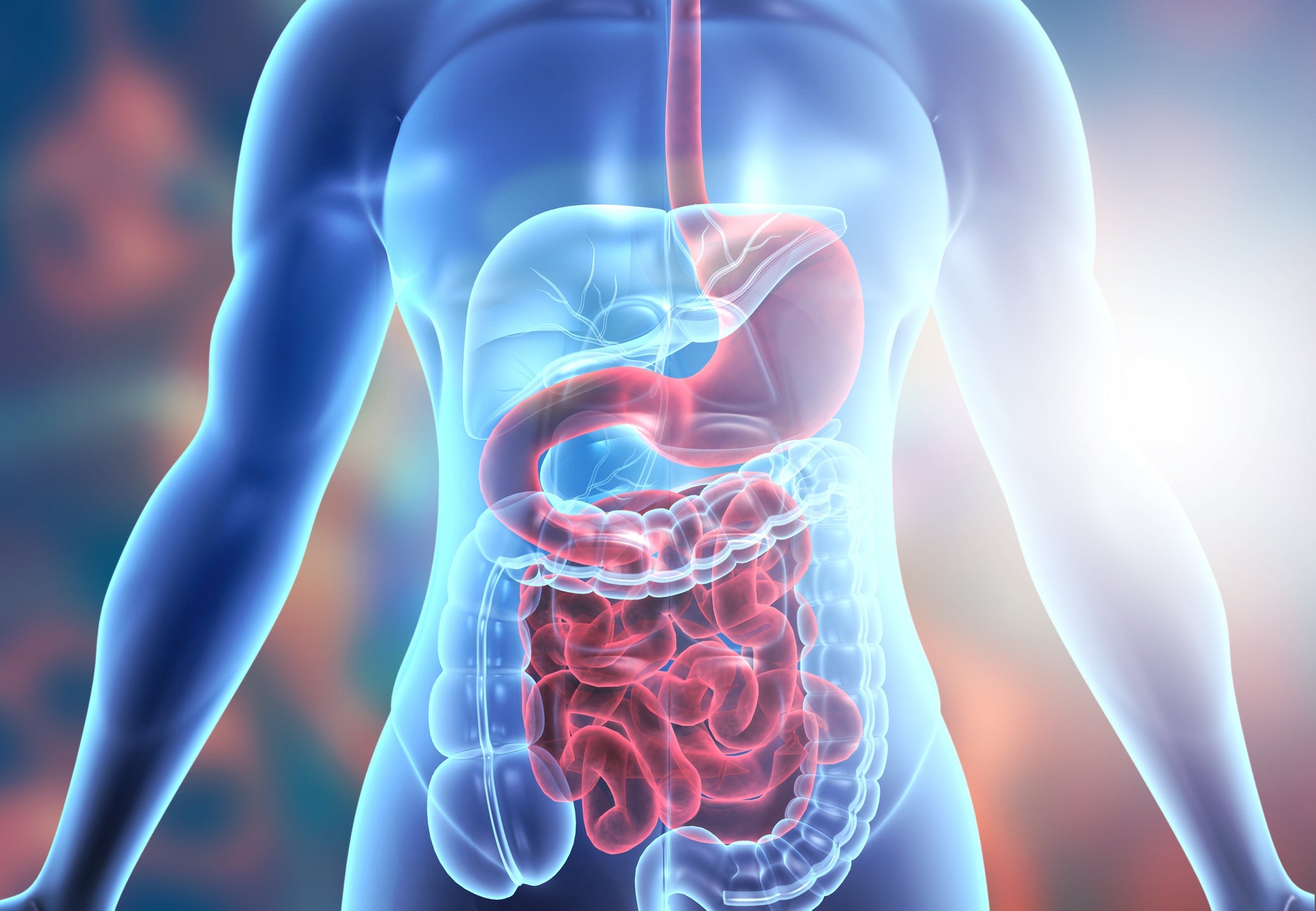
The human gut microbiome is a complex eco-system made up of trillions of bacteria, viruses, fungi and protozoa that live within the intestinal tract, weighing in at around 1.5kg!9 There are in fact more microbial cells in the gut microbiome than there are cells in the rest of the body – hence the state of our gut microbiome significantly impacting our overall health and wellbeing.10
Our gut microbiome is specific to each of us, individually – much like a bacterial fingerprint.11
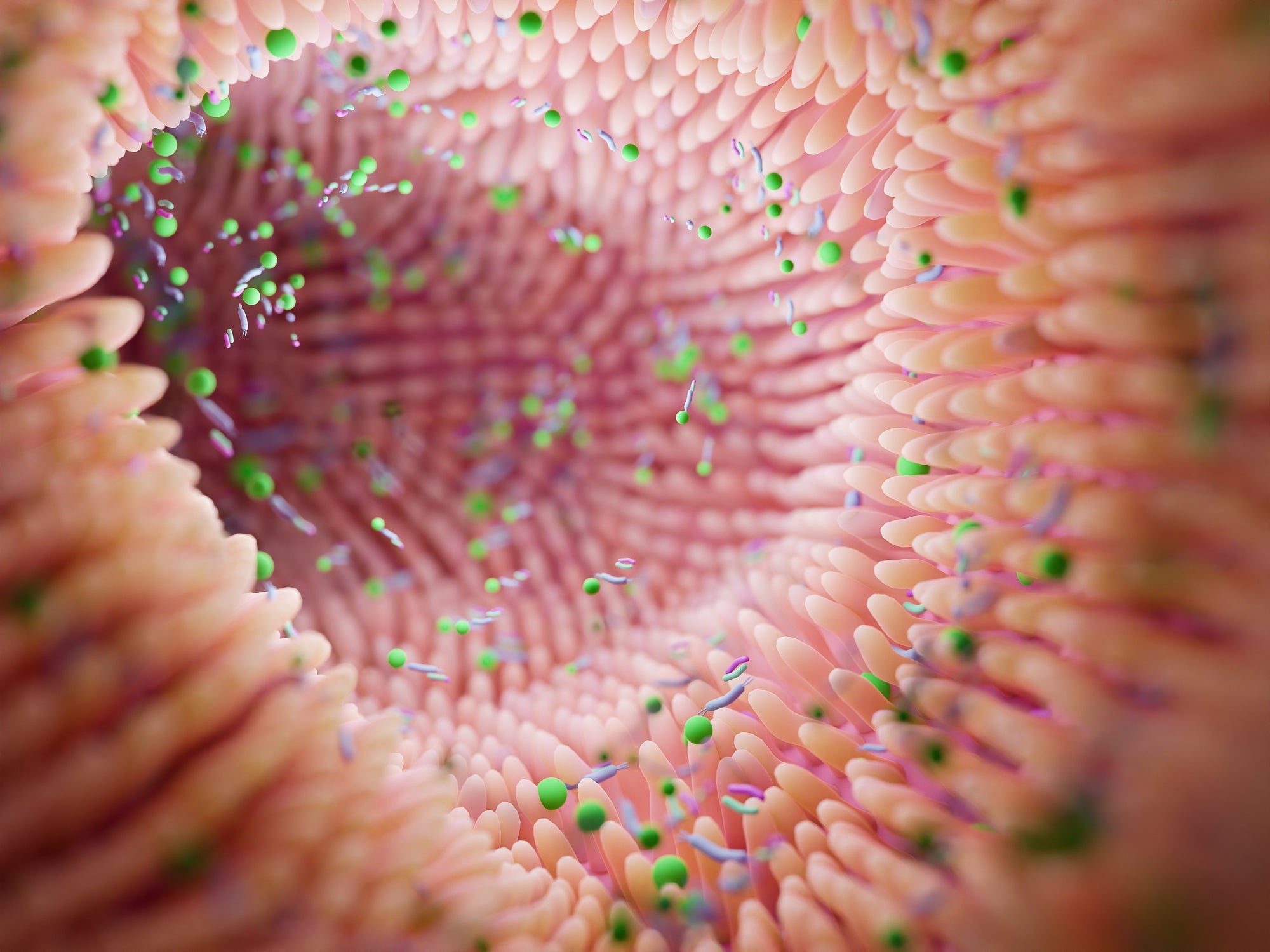
The microbiota (the bugs themselves) together with the gut are collectively known as the enteric nervous system, are often referred to as our “second brain.” This enteric nervous system is so large that it actually contains more nerve cells than are in our spine!12
We begin to populate our microbiome very early in life, with some research suggesting as early as in the womb.13 When we are born, many factors influence the types of bacteria that will live and flourish in our gut. These include the genetics and health of our parents, whether we were delivered vaginally or by caesarean, and if we were breast or bottle-fed.14
Throughout life, many other factors continue to shape the bacteria living in our gut. Some of these are difficult to change, like genetics, stressful events or illness, but some are factors we can modify or control, such as our lifestyle behaviours – particularly our diets.15
A healthy gut will have a robust wall or barrier which keeps its contents, such as the bugs, as well as the undigested food particles and toxins from escaping into the bloodstream.16 Its role is essentially to digest our food, absorb and synthesize the necessary nutrients, excrete toxins and link our digestion, mood and brain health.17 The microbiota also work to help fight off infection, keeping our bodies functioning optimally.
What is the gut-brain axis?
The gut-brain connection is governed by an axis known as the gut-brain axis, which consists of communication between the central and enteric nervous systems, brain and spinal cords, the hypothalamic pituitary adrenal (HPA) axis, and the gut microbiome. This constant communication and signalling occurs through various chemical messengers, the endocrine system and gut hormones as well as via neurotransmitters and helps to keep the body in a state of balance.18,19
Many of these hormones and neurotransmitters, such as gamma aminobutyric acid (GABA), dopamine and serotonin are actually made in the gut, along with gut biproducts of carbohydrate fermentation such as the highly anti-inflammatory short chain fatty acids (SCFA).20
The state of our gut microbiome therefore can regulate our brain and behaviour, influencing normal brain functioning, while a dysbiotic or imbalanced gut microbiome is involved in many psychiatric conditions including depression and anxiety. 21,22,23,24,25,26
The communication between the gut and our brain along the gut-brain axis is bidirectional, meaning one having a profound impact on the other.
The vagus aka “wandering” nerve
Out of the approximately 500 million nerve cells located in our gut, the largest is the vagus nerve - considered a key component of the gut-brain axis. “Wandering” from our brainstem through the neck and the thorax down to the abdomen, our vagus nerve receives information from our gut and transmits it to the brain.27
It is the key component of our parasympathetic nervous system (aka our “rest and digest” system), controlling mood, stress and immune response, hunger and digestion, breathing and heart rate.28
Its signalling and transmission of information from gut to brain relies heavily on our microbiota and also plays a major role in the regulation of inflammation.
Fun fact: Whenever we turn inward to listen to our intuition or become creative or social and are feeling less guarded, this is emotional and psychosocial regulation with thanks to our vagus nerve!29
What happens when our gut-brain axis is compromised?
Both our physical and mental health can be compromised when communication between one or more parts along this axis becomes faulty, such as when dysbiosis or inflammation occurs.30
Stress or trauma also inhibit the vagal nerve function and have negative effects on the gastrointestinal tract and microbiota. Stress and trauma are in fact linked to the development of gut disorders such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) - both characterized by gut dysbiosis.31
3 nutrients to support optimal gut health
Fibre:
An important by-product of fibre digestion is the release of short-chain fatty acids through fermentation. This process lowers the pH levels in the colon which will prevent harmful bacteria, such as Clostridium difficile, from growing. Some high-fibre foods include whole grains, vegetables, fruits, beans, and legumes.32
Prebiotics:
These are non-digestible foods that are beneficial to gut health by acting as a food source for bacteria. Apple pectin, found in our Good Green Vitality formulation is a prebiotic fibre that supports “next-generation” probiotics such as Bacteroidetes. We have also included other prebiotics such as aloe vera and globe artichoke. Prebiotics can also be found in a variety of vegetables (such as asparagus, Jerusalem artichokes, onions, leeks, and savoy cabbage), as well as in legumes, fruits (bananas, watermelon, and grapefruit) and whole grains (like oats and barley).33
Probiotics:
Foods that contain live microbiota promote diverse gut flora.34 This includes yoghurt with live cultures, and fermented foods such as kefir, kombucha, miso, and kimchi. Good Green Vitality also contains Lactobacillus acidophilus and Bifidobacterium bifidum, totalling 8 billion CFUs per serve.
Improving the diversity of our gut microbiome is a gradual process, and consistency is key. Here at Nuzest, we firmly believe that food comes first, however, our fast-paced lifestyles and reliance on convenience foods has meant many of us face detrimental deficiencies in key vitamins, minerals, and antioxidants. Supplementing with our daily and delicious multi-nutrient formula Good Green Vitality can help to fill these nutritional gaps and also provide our friendly gut bugs with the fibre that they love - so they can grow, diversify and improve our gut health! Try mixing Good Green Vitality in a tall glass of water, or in your morning smoothie to support your gut, and essentially, your overall health and wellbeing.
References:
- Holzer P. Gut Signals and Gut Feelings: Science at the Interface of Data and Beliefs. Frontiers in Behavioral Neuroscience. 2022 Jul 5;16.
- Hills RD, Pontefract BA, Mishcon HR, Black CA, Sutton SC, Theberge CR. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients [Internet]. 2019 Jul 16;11(7):1613. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6682904/
- Quigley EMM. Gut bacteria in health and disease. Gastroenterology & hepatology [Internet]. 2013;9(9):560–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983973/
- Koponen KK, Salosensaari A, Ruuskanen MO, Havulinna AS, Männistö S, Jousilahti P, et al. Associations of healthy food choices with gut microbiota profiles. The American Journal of Clinical Nutrition. 2021 May 21;114(2):605–16.
- Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. Journal of Translational Medicine. 2017 Apr 8;15(1).
- Belkaid Y, Hand Timothy W. Role of the Microbiota in Immunity and Inflammation. Cell [Internet]. 2014 Mar;157(1):121–41. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4056765/
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of gastroenterology. 2015;28(2):203–9.
- Carlson JL, Erickson JM, Lloyd BB, Slavin JL. Health Effects and Sources of Prebiotic Dietary Fiber. Current Developments in Nutrition [Internet]. 2018 Jan 29;2(3). Available from: https://academic.oup.com/cdn/article/2/3/nzy005/4828321
- Noce A, Marrone G, Di Daniele F, Ottaviani E, Wilson Jones G, Bernini R, et al. Impact of Gut Microbiota Composition on Onset and Progression of Chronic Non-Communicable Diseases. Nutrients. 2019 May 14;11(5):1073.
- Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Li HB. Impacts of Gut Bacteria on Human Health and Diseases. International Journal of Molecular Sciences [Internet]. 2015 Apr 2;16(12):7493–519. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4425030/
- Quigley EMM. Gut bacteria in health and disease. Gastroenterology & hepatology [Internet]. 2013;9(9):560–9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983973/
- Rao M, Gershon MD. The Bowel and beyond: the Enteric Nervous System in Neurological Disorders. Nature Reviews Gastroenterology & Hepatology [Internet]. 2016 Jul 20;13(9):517–28. Available from: https://www.nature.com/articles/nrgastro.2016.107
- Walker RW, Clemente JC, Peter I, Loos RJF. The prenatal gut microbiome: are we colonized with bacteria in utero ? Pediatric Obesity. 2017 Apr 26;12:3–17.
- Ma J, Li Z, Zhang W, Zhang C, Zhang Y, Mei H, et al. Comparison of the Gut Microbiota in Healthy Infants With Different Delivery Modes and Feeding Types: A Cohort Study. Frontiers in Microbiology [Internet]. 2022 May 26;13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9204251/
- Fülling C, Dinan TG, Cryan JF. Gut Microbe to Brain Signaling: What Happens in Vagus…. Neuron. 2019 Mar;101(6):998–1002.
- Riccio P, Rossano R. Undigested Food and Gut Microbiota May Cooperate in the Pathogenesis of Neuroinflammatory Diseases: A Matter of Barriers and a Proposal on the Origin of Organ Specificity. Nutrients. 2019 Nov 9;11(11):2714.
- Rowland I, Gibson G, Heinken A, Scott K, Swann J, Thiele I, et al. Gut microbiota functions: metabolism of nutrients and other food components. European Journal of Nutrition. 2017 Apr 9;57(1):1–24.
- Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Journal of Clinical Investigation. 2015 Feb 17;125(3):926–38.
- Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain–gut–enteric microbiota axis. Nature Reviews Gastroenterology & Hepatology. 2009 May;6(5):306–14.
- Hamamah S, Aghazarian A, Nazaryan A, Hajnal A, Covasa M. Role of Microbiota-Gut-Brain Axis in Regulating Dopaminergic Signaling. Biomedicines. 2022 Feb 13;10(2):436.
- Foster JA. Gut feelings: bacteria and the brain. Cerebrum : the Dana forum on brain science [Internet]. 2013;2013:9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3788166/
- Hsiao Elaine Y, McBride Sara W, Hsien S, Sharon G, Hyde Embriette R, McCue T, et al. Microbiota Modulate Behavioral and Physiological Abnormalities Associated with Neurodevelopmental Disorders. Cell [Internet]. 2013 Dec;155(7):1451–63. Available from: https://hsiao.science/static/pdf/EYHCell.pdf
- Liu L, Zhu G. Gut–Brain Axis and Mood Disorder. Frontiers in Psychiatry. 2018 May 29;9.
- Liang S, Wu X, Hu X, Wang T, Jin F. Recognizing Depression from the Microbiota–Gut–Brain Axis. International Journal of Molecular Sciences. 2018 May 29;19(6):1592.
- Clapp M, Aurora N, Herrera L, Bhatia M, Wilen E, Wakefield S. Gut microbiota’s effect on mental health: the gut-brain axis. Clinics and Practice [Internet]. 2017 Sep 15;7(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
- Lucas G. Gut thinking: the gut microbiome and mental health beyond the head. Microbial Ecology in Health and Disease. 2018 Nov 23;29(2):1548250.
- Kanai T, Teratani T. [Role of the Vagus Nerve in the Gut-Brain Axis: Development and Maintenance of Gut Regulatory T Cells via the Liver-Brain-Gut Vago-Vagal Reflex]. Brain and Nerve = Shinkei Kenkyu No Shinpo [Internet]. 2022 Aug 1 [cited 2023 Jun 5];74(8):971–7. Available from: https://pubmed.ncbi.nlm.nih.gov/35941793/#:~:text=The%20vagus%20nerve%20is%20considered
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry [Internet]. 2018 Mar 13;9(44). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/
- Wilkie L, Fisher Z, Kemp AH. The Complex Construct of Wellbeing and the Role of Vagal Function. Frontiers in Integrative Neuroscience. 2022 Jul 7;16.
- Góralczyk-Bińkowska A, Szmajda-Krygier D, Kozłowska E. The Microbiota–Gut–Brain Axis in Psychiatric Disorders. International Journal of Molecular Sciences [Internet]. 2022 Sep 24;23(19):11245. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9570195/
- Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience. 2018 Feb 7;12(49).
- Conlon M, Bird A. The Impact of Diet and Lifestyle on Gut Microbiota and Human Health. Nutrients [Internet]. 2014 Dec 24;7(1):17–44. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303825/
- Gagliardi A, Totino V, Cacciotti F, Iebba V, Neroni B, Bonfiglio G, et al. Rebuilding the Gut Microbiota Ecosystem. International Journal of Environmental Research and Public Health [Internet]. 2018 Aug 7;15(8):1679. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6121872/#B69-ijerph-15-01679
- Leeming ER, Johnson AJ, Spector TD, Le Roy CI. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients [Internet]. 2019 Nov 22;11(12):2862. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950569/